In a decision that has ignited controversy and concern amongst Georgia’s most vulnerable residents, Georgia’s Department of Community Health (DCH) has awarded new Medicaid contracts to four insurers—three of which have no prior experience providing healthcare to this population in Georgia.
The move, which reshapes one of the state’s largest public expenses, has raised alarms among patients, providers, and policy experts alike.
The sweeping changes would force more than a million Medicaid recipients to find new health plans, including disrupting health services for foster care children and creating significant gaps in network coverage.
As Georgia prepares to transition an additional 200,000 elderly, blind, and disabled individuals into managed care, critics warn that the state is on the brink of a healthcare crisis. This was covered in-depth by the Atlanta Journal-Constitution before the New Year.
Patient advocates are sounding the alarm about the potentially devastating consequences for Medicaid recipients. With so many Georgians facing the prospect of losing access to their current healthcare providers, many are bracing for delays, confusion, and unmet medical needs.
According to Renu Gupta, the office manager for one of South Georgia’s biggest psychiatric practices, who spoke to the AJC, “It’s not easy to deal with insurance companies, and I’m worried it’s going to be a terrible transition. It’s not fair for the doctors or their practices. And, I’m telling you, these patients are going to suffer for it.”
Hospitals
Local hospitals, particularly those serving rural or underserved communities, are expected to bear the brunt of this upheaval. Burdened with administrative challenges and reduced network access, these medical centers could face financial strain and diminished capacity to provide critical care.
The procurement process behind the new contracts has also drawn sharp criticism, with some labeling it as mismanaged, rife with errors and reckless practices.
Amerigroup, one of the insurers excluded from the new contracts, filed a formal complaint, calling the decision “manifestly not in the best interests of Georgia taxpayers or the Georgians who depend upon Medicaid benefits.”
Insiders familiar with the process have described it as opaque and inconsistent, fueling skepticism about whether the new contracts will deliver better outcomes for Medicaid recipients.
The state’s handling of this high-stakes decision has left many questioning its commitment to ensuring quality care for its most vulnerable populations, and whether unknown and unelected state bureaucrats are best positioned to determine what is in the best interest of the state.
Among those most affected by the overhaul are the 33,000 children and teens in Georgia’s foster care system. These individuals rely on the Georgia Families 360 program, which has been managed by Amerigroup. Critics warn that transferring this program to a new insurer risks significant disruptions in care for children who already face heightened health challenges.
Already underserved markets are bracing to bear the full force of this decision. In Thomasville, for example, Archbold Health System has three locations and a large multi-specialty physician network.
They currently have no letters of intent from new Medicare service providers United, Humana, and Molina, meaning over 10,000 residents will be unable to get the care they need, and will be forced to change providers or travel nearly an hour to get the care they need covered.
This is the same in communities all over the state, including Statesboro, Gainesville, Athens, and even Atlanta's Emory Medical Center.
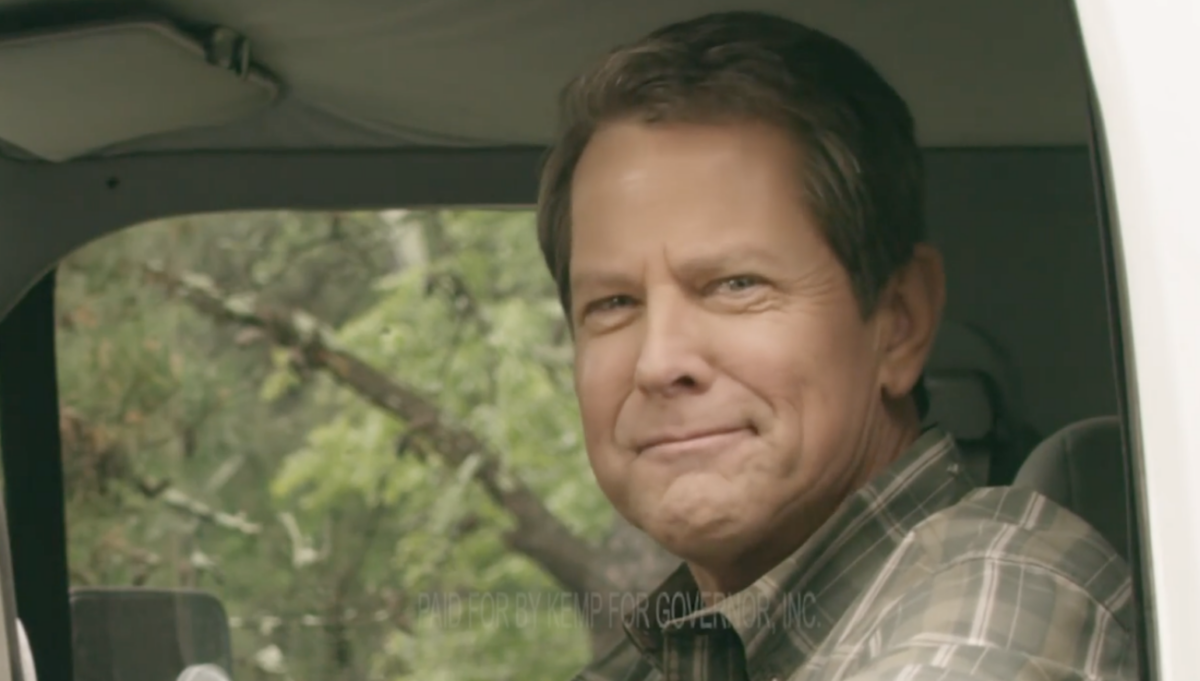
The DCH’s decision comes at a pivotal moment for healthcare in Georgia – a state that already ranks as one of the worst in the nation for healthcare access. With the state’s Medicaid program poised for significant changes, the risks of a poorly managed transition are high. Advocates, healthcare providers, and insurers are urging the Governor and state officials to reconsider their approach to avoid catastrophic disruptions.
For now, the future of Medicaid in Georgia hangs in the balance, with over a million lives and billions of taxpayer dollars at stake.